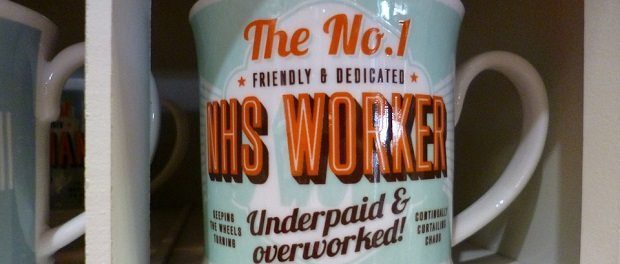
[dropcap style=”font-size:100px; color:#992211;”]E[/dropcap]xtra! Extra! Read all about it! Tory cabinet minister in Being Completely Wrong shocker!
Heavyweight medical-profession journal The Lancet reviews Jeremy Hunt’s proposals for the NHS and, as is apt, clinically slices them apart.
Perhaps a future issue might focus on beginner’s anatomy, particularly the differences between arses and elbows. Free copies to be delivered to Conservative HQ.
The ‘weekend effect’ – that patients admitted to hospital over the weekend are at an increased risk of death – overshadows a much more complex pattern of weekly changes in quality of care, which are unlikely to be addressed by simply increasing the availability of hospital doctors on Saturdays and Sundays, according to two new studies published in The Lancet.
Studies on the weekend effect have had a major, and at times contentious, impact on health policy. Policy makers, including the UK Secretary of State and Department of Health have explicitly attributed the weekend effect to reduced availability of hospital doctors at the weekend, concluding that changes to doctors’ employment contracts will be required to deliver high quality care seven days a week. So far, however, evidence about the quality of care at the weekend compared with weekdays, or whether there is a direct link between mortality and the availability of consultants remains largely speculative.
The first paper, led by the University of Birmingham, UK, finds no association between weekend senior doctor staffing levels and mortality. While the second paper, led by King’s College London, and University College London, UK, looking specifically at acute stroke care, finds no weekend effect on survival, but reveals there are many variations in quality of care throughout the week, and that policies to address weekend quality of care alone represent a major oversimplification of the problem.
The two papers add evidence to a report published last week suggesting that weekend mortality differences might be attributable to how sick patients are on admission, rather than the quality of their care.
In the first paper, researchers from the High-intensity Specialist Led Acute Care (HiSLAC) project led by the University of Birmingham collected data on senior doctor input into emergency admissions at 115 NHS trusts at two time points – Sunday 15th and Wednesday 18th June 2014.
Hospital consultants completed a survey recording the number of hours they spent between 8am and 8pm caring for patients who had been admitted as an emergency. A similar survey was completed by clinical service directors and the findings were compared to national hospital mortality data.
There were substantially fewer senior doctors present and providing emergency care on Sunday (1667) compared to Wednesday (6105). This was partly offset by the fact that doctors spent on average 40% more time caring for emergency admissions on Sunday (5.74 hours) compared to Wednesday (3.97 hours). Once the total number of admissions per hospital was taken into account, the findings show that emergency admissions on a Sunday collectively receive on average less than half the input of senior doctors compared to patients admitted on Wednesday (21.90 total specialist hours per ten emergency admissions on Sunday; compared to 42.73 hours on Wednesday) .
The researchers then looked at average weekend mortality data for all 115 trusts for 2013-14. On average, there was a small increase in the risk of death associated with weekend admission (10% relative risk increase on weekends compared to Wednesdays), but mortality differed between trusts. When mortality risk was plotted against senior doctor staffing levels, there was no evidence of an association between the two. .
“Patients admitted to hospital over the weekend are likely to receive less time with consultants, and do indeed have a slightly higher risk of death. Both problems need to be addressed to provide consistent standards of high quality care. But to say that lower staffing is the cause for increased mortality is far too simplistic and not supported by the evidence,” says lead author Professor Julian Bion, University of Birmingham. “Policy makers should be extremely cautious when attributing the weekend effect directly to the lack of consultants at the weekend.”
The authors warn that the study is part of a longer term project and that finding a lack of association now cannot discount it in the future. The study did not include data on staffing of junior doctors, nurses or information about how ill patients were. Nevertheless, the authors urge caution in linking mortality directly to senior doctor staffing levels, and say that more research is needed to understand the key factors affecting mortality in such a complex system.
The second study, led by researchers at King’s College London and University College London, looked at how the quality of acute stroke care in particular varies by day of the week and time of day, over a whole year. The study included care data from 74307 patients admitted to 199 hospitals in England and Wales between April 2013 and March 2014, and information about patient survival 30 days post admission.
There was no difference in 30 day survival for patients admitted during the day at the weekend, compared to during the week, and only very weak evidence that survival was worse for patients admitted overnight compared to those admitted during the day.
The researchers found there was wide variation in the quality of care delivered – both by days of the week and time of day. Patients who arrived in the morning were more likely to receive a brain scan within one hour (as per national stroke care guidelines ) than those who arrived in the afternoon; patients admitted on a Monday had the lowest odds of being admitted to a stroke unit within four hours; and patients admitted on Thursdays and Fridays experienced the longest waits for therapy assessment.
“Much of the current discourse on reducing the weekend mortality effect has occurred in the absence of a detailed understanding of why changes in quality of care occur. Our study shows that the ‘weekend effect’ is a major oversimplification of the true extent and nature of variations in the quality of care that occur in everyday practice. Our findings apply to stroke care in particular but are likely to be reflected in many other areas of health care,” says lead author Dr Benjamin Bray, from the Royal College of Physicians’ Clinical Effectiveness and Evaluation unit and University College London.
“When solutions come at such a high financial cost, it is imperative that policy makers, health-care managers and funders base their decisions on evidence. Simply transferring doctors from weekdays to weekends is highly unlikely to have the intended effect of improving quality of care.”
Commenting on all three recently published papers, Professor Nick Black, London School of Hygiene & Tropical Medicine, London, UK, points to many factors that may help explain the increased risk of mortality at the weekends, not least that patients are sicker, and says more research is needed that focuses on other outcomes and patients’ experiences.
He concludes: “Despite many claims about the quality of care at weekends and strong beliefs about the reasons for this, we need to remain open to the true extent and nature of any such deficit and to the possible causes. Jumping to policy conclusions without a clear diagnosis of the problem should be avoided because the wrong decision might be detrimental to patient confidence, staff morale and outcomes.”
Source: Eurekalert/The Lancet

Some of the news that we find inspiring, diverting, wrong or so very right.